Evolution is the fundamental idea in all of life science – in all of biology
Bill NyeLife sciences encompass a range of knowledge that touches on very different aspects. The basis is biology, the study of physical and chemical processes that characterise living systems. From this, come fields of application such as biochemistry, molecular analysis, genetics, physiology, up to emerging processes that regulate development and adaptation, the assessment of behaviour and the interaction between organisms.
In Italy, biomedical engineering is an area of real excellence in the healthcare world. This intricate work sector includes subjects such as mathematics, chemistry, physics, biomechanics, materials science, electrophysiology, neurophysiology, cognitive sciences and the cybernetic field, such as in bio and nanotechnologies. With an engineering technical and design approach, it is possible to study effective solutions and systems for the biomedical sciences. Starting with the definition of a problem from a medical-biological point of view, engineers build artificial organs and prostheses, and develop electro-medical equipment for diagnosis, treatment and rehabilitation.
Biomedical engineering is also involved in organising hospital departments, compliance with safety regulations relating to medical devices and acquiring and processing data in the field of diagnostics and monitoring.
Biotechnology is a complementary field to biomedical engineering. In this area, which is more directly linked to research and development activities, biotechnological investigation method techniques and the use of laboratory equipment are focussed on designing products for the chemical-pharmaceutical industry. Microbiological, biochemical and genetic analyses and toxicology checks allow for drug experimentation and development. The ability to use and manage innovative software for collecting, documenting and drafting complex reports is one of the biotechnology research management activities.
Healthcare is one of the most dynamic industrial sectors and in recent years has undergone a real revolution thanks to a series of technological evolutions and innovations that are reshaping the future. In particular, this profound transformation has impacted products for patient care and at the same time the dynamics and working rules for doctors. Together, these two inputs have generated new business models for the entire sector.
But what are these instruments that are revolutionising healthcare? They include telemedicine and artificial intelligence, digital-health Clinical Decisional Support Systems (CDSS), virtual environments and computational approaches, blockchain to track the health of patients, and personalised and precision medicine. The virtuous chain that has led to this involves a demand for continuous innovation, followed by huge investments in the Research & Development sector and finally the resulting solutions applied to the medical field.
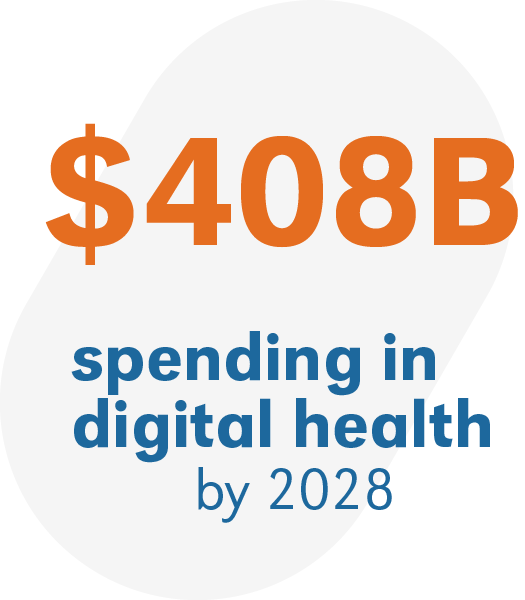
The focus on this issue is not limited to companies in the healthcare and biopharma sectors of expertise, but inevitably extends to the big technology players, Google, Microsoft and Apple above all. The figures coming out of some recent reports highlight this dizzying interest and predict the spending in R&D for companies in this sector will grow to over $408 billion dollars between now and 2028.
The medical device industry in the world
With a global spending in Research and Development (R&D) estimated at around $300 billion in 2022 and an R&D expenditure-to-revenue ratio among the highest (12.61%), the Life Sciences sector represents a crucial area for innovation and the development of new technologies. These figures outline a significant development area for Teoresi Group, especially considering that R&D expenses in the entire Life Sciences sector also record an average annual growth of 4.8% for the period 2023-2028. The sector is divided into three main segments: Pharma, MedTech (Medical devices), and IVD (In vitro diagnostic medical devices), each with specific dynamics. The MedTech segment, in particular, closely aligned with Teoresi Group’s expertise, is experiencing significant growth, with a CAGR of +6.1%, and is the most expansive with a global R&D spending of approximately $30 billion in 2022. The medical devices sector encompasses a wide range of instruments and machinery that support healthcare providers in the prevention, diagnosis, and treatment of diseases, including cardiology devices, diagnostic imaging, orthopedic devices, ophthalmic, general and plastic surgery devices, as well as AI-based medical devices, augmented/virtual reality, robotics, IoT, and telemedicine devices. This landscape provides Teoresi Group with a fertile ground to expand its scope of expertise and offer innovative and technologically advanced solutions in the Lifescience sector.


In its national guidelines, the Italian Government’s Ministry of Health provides the definition of Telemedicine as „meaning a way of providing healthcare services, through the use of innovative technologies, in particular Information and Communication Technologies (ICT), in situations where the healthcare professional and the patient (or two professionals) are not in the same place. Telemedicine involves the secure transmission of medical information and data in the form of text, sound, images or other forms that are necessary for prevention, diagnosis, treatment and subsequent monitoring services for patients. Telemedicine services must be in line with existing diagnostic/therapeutic healthcare services“. The definition goes on to specify that telemedicine does not in any way replace the traditional healthcare service, and the related personal doctor-patient relationship, “but is integrated with it to potentially improve its efficacy, efficiency and appropriateness. Telemedicine must also comply with all the rights and obligations under any healthcare act“.

By 1997, the WHO (World Health Organization) had already defined how it should look. „The delivery of healthcare services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities“.
The global pandemic starting at the end of 2019 linked to COVID-19 (see FOCUS) has made the need for a radical change in medical care even more urgent.
Telemedicine has different healthcare purposes:
| Improving the quality of healthcare |
| Enabling improved usability of care and diagnostic services |
| Allowing for remote medical advice |
| Allowing constant monitoring of vital signs and therefore of the state of health of patients |
| Reducing the risk of complications in people at risk or suffering from chronic diseases. |

In relation to the social fabric, telemedicine gives administrative areas the possibility to increase equity of access to social and healthcare services, especially for those who are geographically isolated, thanks to the service’s flexibility of delivery and use. In this way, continuity of assistance in the area is guaranteed, at the same time allowing resources to be allocated where they are most needed, without wasting valuable professional time on simple physical supervision. Finally, teleconsultation can offer significant support to emergency mobile services, with the use of remote clinical resources, even directly on board ambulances.

Telemedicine, COVID-19 and post-pandemic
Terms such as „monitoring“ and „distancing“ have become familiar when talking about health protection, particularly following the spread of the COVID-19 virus from the end of 2019. Apps to track people’s movements and the need to manage discharged or asymptomatic patients with telehome methods, if not fully resolving issues, have put them at the centre of the debate.
Telemedicine is also very effective in preventing the collapse of emergency service management, as was observed above all during the early months of the spread of the pandemic. For example, for asymptomatic positives, it allowed us to measure the parameters we learned were the most evident manifestations of the virus infection and its most aggressive. These include above average body temperature, respiratory rate and oxygen saturation, and heart rate related to respiratory rate. Home monitoring can help with taking prompt action where the condition worsens. Similarly, it is advisable to continue monitoring patients after they are discharged, since they are considered recovered, the aforementioned parameters in the full recovery stage can then be observed.
Another issue dramatically brought to the fore throughout 2020, was the care of patients with emergencies not related to COVID-19. With intensive care units at full capacity, it was not possible to treat cases such as heart attacks in a timely and appropriate way. Monitoring of this category of patients is also essential when the relationship between hospital and patient is rendered impossible for various reasons. In general, the emergency accelerated the transformation of telemedicine from an emergency tool to one used routinely.
The Life Sciences sector is growing rapidly. The relationship between treatment and disease, between doctor and patient is heading for a radical change. The next challenge is the transition from the traditional medical approach to 4P medicine.

Predictive : with diagnostic processes and cutting-edge technological tools, it is possible to prevent diseases and limit their effects.
Preventive: to support and promote adequate prevention processes with a specific focus on the individual’s well-being.
Participatory: where the patient can interact, discuss and choose what action to take following the logic of prediction and prevention.
Personalised: to respond in the most detailed and effective way possible to the physical, physiological and clinical characteristics of the patient.
In 2013, the world of digital information already stood at around 98% of all information produced globally. In healthcare, the annual growth rate of generated data has reached 48%. Medical records are often include videos, images, texts and audio files that support research of the patient’s clinical profile. In the same way, increasingly advanced diagnostic programmes go hand in hand with the affirmation of BigData and IoT, opening up the possibility for everyday objects such as clothing, smart home systems, vehicle technology and smartphones to collect data on the health of the body, such as heart rate, glucose levels, blood pressure, body temperature and then transmit this crucial information via the internet.
BigData has put the delicate issue of data processing and analysis at the centre of the debate. Thanks to a new research approach, with cognitive analytics and machine learning systems, algorithms can process an impressive amount of data, but in order for it to have value and be readable to extract valuable information, it is necessary to refer to the skills of data science specialists. Precision medicine, used in diagnosis, will increasingly encourage the use of in-depth sectoral knowledge to treat diseases, prevent epidemics and improve people’s quality of life and life expectancy. The 4 P’s are, indeed, the objectives to aim for.
Medicine is changing rapidly. From a system focussed on disease management to a molecular and systemic approach typical of systems biology, which studies living beings as structures in evolution. In particular, we are trying to understand genomics better to evaluate the dynamic system changes. From mathematics-statistics to bioinformatics, up to biomolecular disciplines, the idea is to collect the digital behaviours of patients and users, and to work with the data for a preventive purpose. Technology’s continuous growth is the additional tool which will make this possible.

Prompt intervention in an emergency situation can play a crucial role in a patient’s health. Teoresi’s in-house design is based on a combination of AI systems with health diagnostic systems using imaging and forecasting and AI analysis to support health assessments, monitoring patients‘ vital signs. Applying this technology to a continuous mobile assistance system during sporting events or emergency situations guarantees more efficient monitoring and rapid support.

A software platform which reproduces the workings of at least 2 primary organs connected to each other, to test drugs currently in clinical use for applications other than those for which they are currently on the market. The idea involves the creation of a remotely accessible software platform that is User friendly – end to end, implemented with tools approved by government bodies. It is an expandable computational model that can be extended to cover more functions and organs.

The project (NANOCAN) is based on the development of a medical device prototype through the study, design and integration of HW and SW platforms for theranostic applications (a combination of diagnostic and therapeutic functions), to carry out joint and sequential diagnostic and therapeutic treatments in real time for breast cancer and liver cancer. The project is aimed at liquid biopsy, spectroscopic imaging for developing tissue biopsy functionality without biological sampling and controlled release of drugs on site.

The research activity has led to the design and development of a low-cost tele-rehabilitation platform based on artificial intelligence capable of suggesting cognitive and motor rehabilitation exercises and monitoring their performance over time through the use of a common RGB camera.
Furthermore, preliminary studies conducted on a heterogeneous cohort of volunteers have allowed the evaluation of the platform’s performance.

The project focuses on the development of an augmented reality (AR) training system – AR Suture Training – designed to enhance surgical education through the integration of advanced immersive technologies, both software and hardware. Its aim is to improve practical learning for medical students and young professionals, enabling them to refine suturing techniques in a realistic and interactive environment, without operating on real patients. The system offers features such as virtual anatomical models generated from CT scans, interactive guidance throughout the incision and suturing process, and real-time feedback to track accuracy and progress. A later evolution of the project introduced a virtual reality (VR) version, which further enhanced the fluidity and immersiveness of the training experience.
